Designing Healthcare Facilities for Infectious Diseases (I) - Medical Planning

Over the last couple of decades, infectious diseases seem to be evolving, requiring different forms of treatment and containment procedures. Highly infectious diseases are mostly viral and bacterial infections that are easily transmissible from person to person, cause a life-threatening illness with no or few treatment options, and pose a threat for both personnel and the public. Thus, with every infectious disease outbreak, the preparedness of the healthcare sector is put to test.
In healthcare settings, early detection of infectious diseases plays a crucial role in all treatment and prevention strategies. An infectious disease facility should be designed to be able to screen, isolate, and treat patients with different types of infectious diseases, while having the flexibility to be adapted in future for different forms of treatment, all the time remaining functional and friendly for use by staff and patients.

National Centre for Infectious Diseases (NCID), Singapore
At CPG Consultants, our Healthcare Division’s experience with medical planning and designing for infectious diseases facilities is extensive. In the past, we designed isolation rooms for major hospitals in Singapore such as the Singapore General Hospital, National University Hospital as well as Changi General Hospital just to name a few. At the height of the SARS crisis in 2003, the Singapore Ministry of Health requested CPG to put together additional isolation facilities for SARS patients on the open grounds of the Communicable Disease Centre (CDC) in Tan Tock Seng Hospital (TTSH), as well as renovate the old buildings on TTSH premises.
It is important to ensure that the design of an infectious disease facility will help to allow for measures of isolation of suspected cases for investigation and management to be done swiftly and effectively. Infectious diseases could be airborne, or spread by droplets or by contact of blood or body fluids. They can be spread person to person, or indirectly, through a medium, via a carrier or transmitted by contact with a surface which has been contaminated by another person. Careful medical planning of the facility in terms of workflow and adjacencies is critical to ensure safety of patients, visitors and staff.
Patient Room Designs
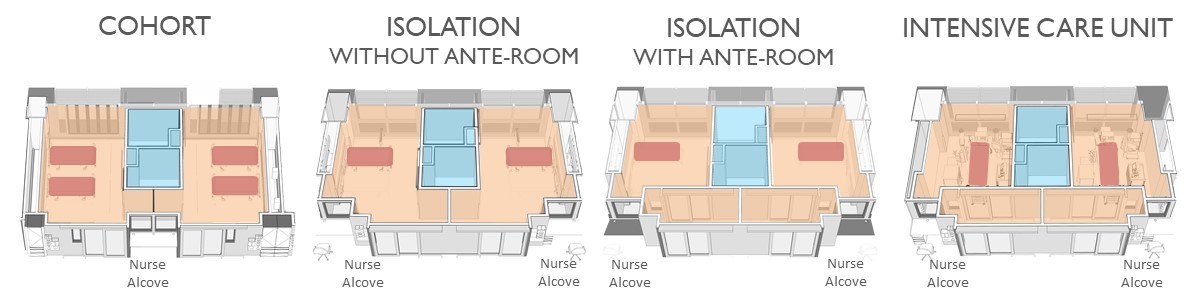
A common type of template for different patient rooms
An infectious health facility should be designed to provide appropriate isolation and intensive care units for inpatient care. Four types of patient rooms (Cohort, Isolation room with no ante-room, Isolation Room with ante-room and Intensive Care Unit) are designed based on a modular template, with similar sizes and similar toilet cores regardless of the type of patient room. This makes it easier to convert from one room type to another in future should the need arise. For example, if more rooms with ante-rooms are needed, renovation would be much easier with rooms based on a modular template, than if the room structures were very different to begin with. Every room has also to be tested for air-tightness at the completion of construction.
A Cohort room with 4 beds in the same room is designed to be naturally ventilated and can house patients with the same infection. This could be a case of family members or patients of the same gender. This design is more space efficient as it houses more patients (four patients instead of two) if they were single-bed rooms. In most cases, patients in 4-bedder Cohort rooms are also less ill, and by gathering them in the same area, helps save on staffing resources.
The typical Isolation Room (without ante-room) is designed to house a single patient who is more infectious than those in the 4-bedder Cohort room. Negative pressure and single-pass air conditioning in the room aim to reduce the risk of infection to other people. When CPG Healthcare team was working on the National Centre for Infectious Diseases [NCID] (a 330-bed purpose-built facility inaugurated in 2019 to strengthen Singapore’s capabilities in infectious disease management and prevention) project, we initiated an improved design where instead of the traditional design of having the toilet closer to the ward corridor, the design includes a maximum glass frontage from the ward corridor, in order to allow staff to supervise the patient.
Isolation rooms with ante-rooms are similar in design, with the addition of an ante-room, to house patients with even more highly contagious or air-borne diseases. An ante-room serves to control contaminated air. Upon leaving the patient room, one enters the anteroom which is a negative air environment. This means that the air in the patient room cannot flow out into the ward corridor outside. Medical workers can also remove their personal protective equipment (PPE) here so that it doesn’t contaminate areas outside of the patient room.
In normal hospitals, the Intensive Care Unit (ICU) do not come attached with ante-rooms if there is no need to handle infectious patients. For an infectious disease facility however, the ICU would have to come with ante-rooms not only to cater to severely infectious patients who are critically ill and need more medical support, but also to ensure infection doesn’t spread. In a certain type of ICU design which CPG devised, we introduced the additional design feature of a pass-through hatch between the ante-room and the patient room. Supplies can then be passed without the need for a staff to enter the room, thus reducing the exposure of staff to infectious patients.
High Level Isolation Unit (HLIU)
In addition to the Cohort, Isolation and ICU rooms mentioned, for patients with infections that are highly virulent and can be spread from person to person, a special type of “High Level Isolation Unit” (HLIU) ward can provide the best care for patients of this nature. During the Ebola outbreak, the CPG Healthcare team had visited hospitals in USA which handled Ebola cases to study the requirements needed. Subsequently, we conceived the HLIU design.
The HLIU unit consists of:
- The patient room with ensuite toilet and shower
- A clean donning room for staff
- The dirty doffing room together with staff shower
- A Dirty Utility room
- A viewing area outside that can be used by staff, or for the patient’s family member
The HLIU unit is also designed to manage staff flow, patient flow, visitor flow and material flow so that cross contamination can be avoided.
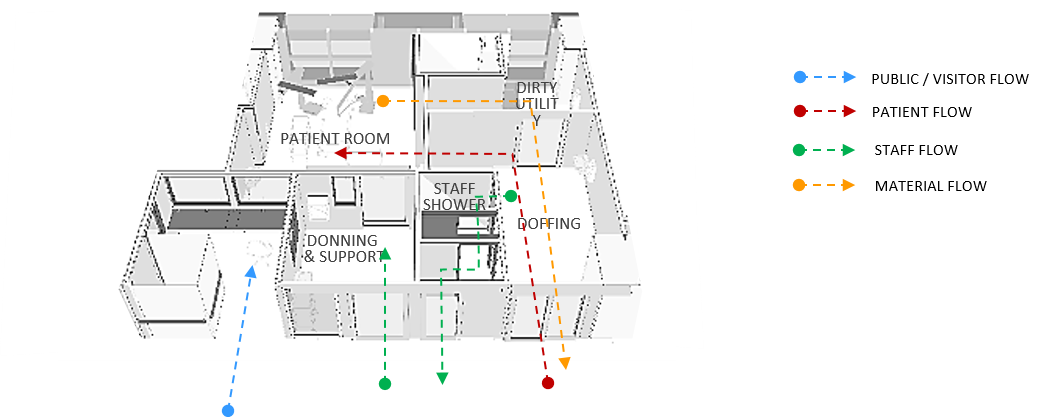
Example of a High Level Isolation Unit (HLIU) design
Staff Flow: Staff would already have put on their first level of PPE when they enter the ward. Before entering the patient room, there is a clean area to don additional PPE (Donning & Support room). Typically, staff serving the patient would stay in the patient room for a few hours. If they need additional supplies, these can be passed to them via the pass-thru hatch. When staff exit the patient room, there is a separate “Doffing” room where they can remove the outer PPE, then enter the staff shower area and put on clean PPE before returning to the ward.
Material Flow: All equipment is brought into the Dirty Utility room and cleaned before leaving the unit. Patient waste will be treated with chemical, double bagged and put into bins before being brought out. They will subsequently be brought to the decontamination area to be autoclaved before leaving the ward.
Patient Flow: Patients are masked and protected, and are wheeled into the HLIU via designated routes which would be decontaminated immediately. After the patient is brought into the patient room, the trolley would be decontaminated in the Dirty Utility Room before being brought out into the ward.
Visitor Flow: While visitors are not encouraged due to the risk of infection, research evidence has shown that patients recover better with the presence of their loved ones. Therefore, in order to accommodate visitors yet ensure their safety, patient and visitor routes are separated clearly. Patients are brought into the patient room via the doffing room. Visitors (restricted) will be permitted to enter the ward and communicate with the patient through a viewing window.
Designing of Rooms for Convertibility
Rooms are also designed in a way that during an escalated outbreak, the number of beds can be increased flexibly to house additional patients with the same illness. Medical gases and other support facilities have been designed to take care of the additional patients. With flexibility in these designs, it is estimated that the number of beds can be increased by 30-40% during a major outbreak.

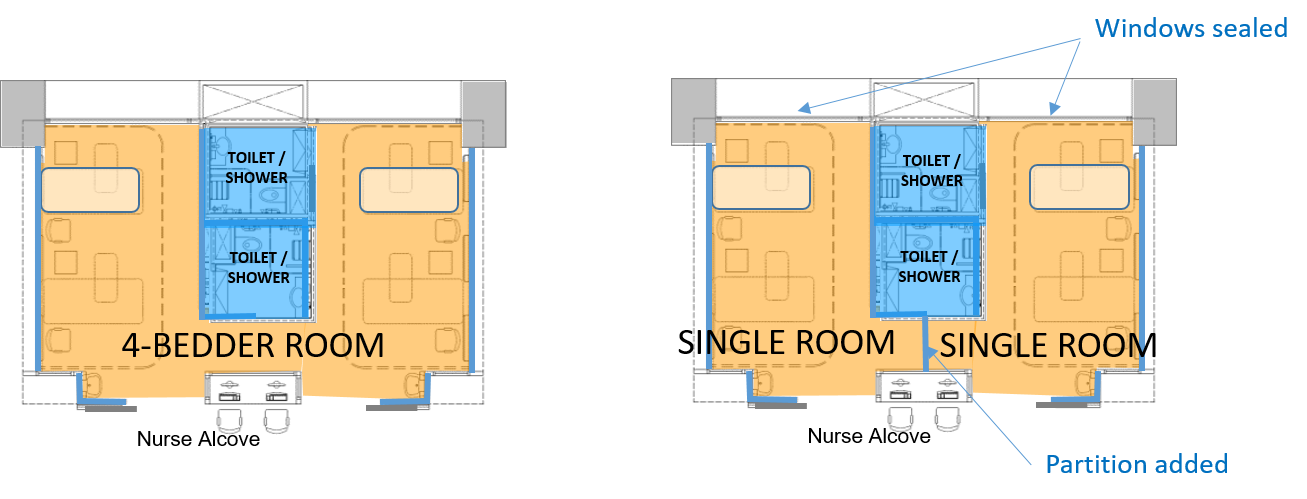
Converting Cohort to Single Isolation Room
In addition to designing for accommodating an increase in number of beds, rooms types can also exercise convertibility. A 4-bedder Cohort room which is designed to be naturally ventilated can be converted to two Isolation rooms by installing a partition, closing and sealing the windows and air-conditioning the room (with checks to ensure the designed air pressure is achieved).
Convertibility not only helps an infectious disease facility deal with major outbreak situations but will also make it more economically viable for it to function when it's required to switch between modes of use. Take for instance the NCID which had adopted CPG Healthcare team's room designs. In a Straits Times article (published 7th Sept 2020) highlighting NCID's battle against the COVID pandemic, it was said that "the magnitude and speed of its spread were unprecedented..." and the facility had to expand its capacity quickly. "...Fortunately, NCID's design allowed for it to be scaled up should the need arise."
In a nutshell, infection control in a health facility is imperative in maintaining a safe environment for everyone by reducing the risk of the potential spread of disease. Medical planning as part of an important strategy used under infection control should consider room designs that can increase bed count flexibly, effectively isolate patients for treatments, provide adequate staff support facilities, as well as facilities, which can be adjusted to cater for new medical protocols in future.
These planning considerations when combined with well-trained healthcare workers, effective mechanical systems and adherence to strict medical protocol befitting outbreak situations, can help to achieve a more optimal environment for patient care which will help more people embark on the journey to recovery. Every infectious disease outbreak will bring about new challenges, but a well-designed infectious disease facility will provide the foundation necessary to meet these challenges.
By Ruby Lai, Senior Consultant, CPG Consultants
Reference:
Salma Khalik (2020) “Battle with Covid-19 a baptism of fire for NCID”, The Straits Times, 7 Sept 2020. Available at https://www.straitstimes.com/singapore/health/battle-with-covid-19-a-baptism-of-fire-for-ncid (Accessed 7 Sept 2020)
-----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
This blog post is the first part of a two-part series introducing CPG Consultants’ experience with specialised healthcare facilities designed to handle infectious diseases. You may also like to read "Designing Healthcare Facilities for Infections Diseases (II) - Engineering Designs for Safety" .
COVID-19 has transformed much of the way we live. How can our built-environment be more pandemic-resilient?
Read more at our special section for insights on a pandemic-resilient BE by our multi-disciplinary experts.



